“How one tragic flight led to a worldwide revolution in trauma care”
✈️ The Crash That Changed Trauma Medicine
It was the evening of February 17, 1976, when Dr. James K. Styner, an orthopaedic surgeon and experienced pilot, was flying his Beechcraft Baron aircraft back home after attending a wedding in Los Angeles. His wife, Charlene, and their four children were aboard. As they traversed the vast expanse of rural Nebraska, deteriorating weather conditions forced Dr. Styner to fly at a lower altitude to maintain visual contact with the ground. Tragically, the plane collided with a row of trees at approximately 168 miles per hour, crashing into a cornfield near Hebron, Nebraska.

What followed was an experience that would deeply shake his faith, not in aviation or fate, but in the medical system he was part of.
💔 The Aftermath: Survival Against the Odds
The crash had devastating consequences. Charlene was ejected from the aircraft and killed instantly. Dr. Styner sustained serious injuries, including rib fractures and facial trauma. His ten-year-old son, Chris, suffered a fractured forearm and severe hand lacerations but remained conscious. Together, despite their injuries, Dr. Styner and Chris managed to extricate the other three children—Randy, Rick, and Kim—all of whom were unconscious with critical head injuries.
In sub-freezing temperatures, Dr. Styner left the crash site to seek help. After walking nearly a mile, he flagged down a passing motorist who transported the family to the nearest hospital in Hebron.
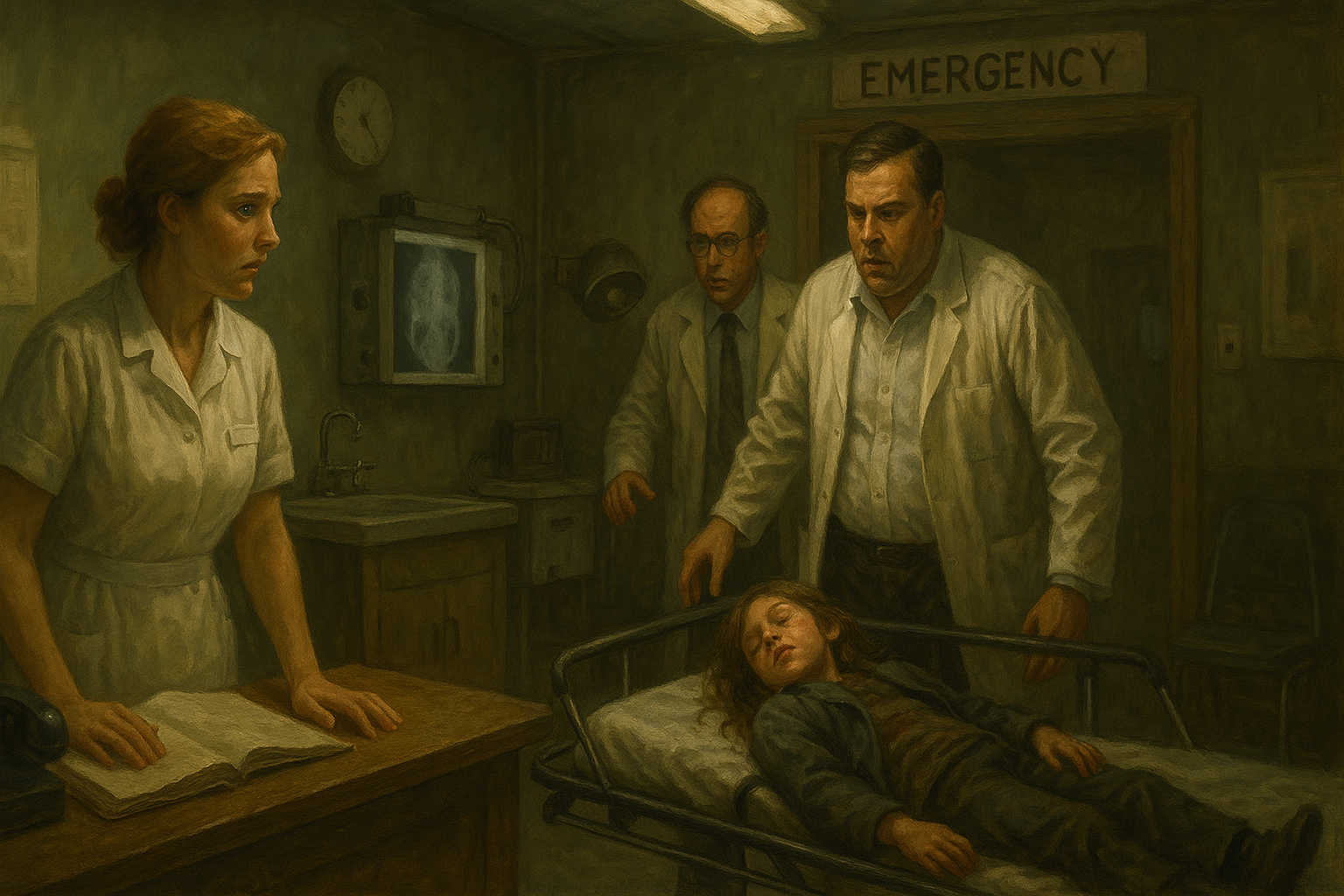
🚑 A Broken System: Trauma Care Before ATLS
The nearby rural hospital in Hebron had an emergency room, but it was closed. A lone nurse on duty, visibly panicked and untrained in trauma care, called two general practitioners: Dr. Pembry and Dr. Bunting. They arrived quickly, but it became clear they were just as overwhelmed and unprepared.

One of Dr. Styner’s sons, Richard, showed signs of head trauma and agitation. He was carried, without spinal immobilisation, to radiology for a skull X-ray. The doctors, relieved to see “no fractures,” ignored the spine entirely. In 1976, CT scans were rare, especially in rural hospitals. Basic trauma principles like ABC assessment or cervical stabilisation were simply not standard practice.

Dr. Styner later reflected:
“I realised I gave better trauma care in that cornfield with a flashlight than what we received in the hospital.”
Unable to watch this any longer, he called his friend Dr. Bruce Miller in Lincoln. What followed was the first civilian helicopter rescue operation in that region, arranged by the Lincoln Air National Guard. Fourteen hours after the crash, the Styner family was flown to Lincoln Hospital, where a surgical team took over.

Miraculously, all of Dr. Styner’s children survived. But the experience left an indelible mark.
🧠 A Vision Born from Pain
As Dr. Styner recovered—physically and emotionally—he began to reflect not only on the accident, but on the chaos and lack of structured trauma response. What if this happened to someone who wasn’t a doctor? What about other rural hospitals?
With Dr. Paul “Skip” Collicott and the Lincoln Medical Education Foundation, he began building a structured trauma course, drawing on lessons from Advanced Cardiac Life Support (ACLS).
But there was another crucial voice in the room.
👨⚕️ Dr. Ronald Craig: The Voice of Rural Medicine
Dr. Ronald Craig, a family medicine physician, understood firsthand the pressures rural doctors face. They are often the first (and only) responders in emergencies. He insisted that any trauma system must be usable by generalists, not just surgeons.
“You have to train them before you can blame them,” Craig said.
His input helped shape the course into something accessible, standardised, and realistic for any setting.
🎓 The First ATLS Course

The first Advanced Trauma Life Support (ATLS) course was held in Auburn, Nebraska, in 1978. It taught a simple yet revolutionary concept: a step-by-step approach to managing trauma.
The mantra was:
- Airway
- Breathing
- Circulation
- Disability (neurological status)
- Exposure (and Environment)
By 1980, the American College of Surgeons Committee on Trauma (ACS-COT) adopted ATLS, and its impact quickly rippled across the United States and the world.
What began in a snow-covered cornfield is now part of every trauma doctor’s foundation.
🩺 Final Thoughts
Dr. Styner turned an unspeakable tragedy into a worldwide movement. His story is not only about grief and survival, but about courage, accountability, and vision.
He taught us that medicine cannot rely solely on good intentions—it must be systematic, teachable, and replicable.
Because trauma doesn’t wait, and lives depend on what happens next.
This blog post is dedicated to the legacy of Dr. James Styner, Dr. Ronald Craig, and the countless trauma teams worldwide that continue to carry forward ATLS’s mission.