“Sometimes, healing is not about curing, but comforting, understanding, and standing beside someone in their most vulnerable moments.”

Every ICU has its share of silent battles—some won, some lost, and some that leave behind stories of courage, endurance, and acceptance. This is one such story.
The Beginning of an Unexpected Journey:
A man in his late sixties arrived at our facility in visible distress—his face etched with pain, his voice strained as he described a sudden onset of excruciating abdominal pain, swiftly followed by relentless bouts of vomiting. From the first moment, it was clear: this was no routine gastritis or food poisoning. The symptoms hinted at something more sinister—an underlying pathology that demanded immediate attention.
A Race Against Time:
We knew we had to act fast. The signs were unmistakable—rigid abdomen, rebound tenderness, fever, and an escalating heart rate. He was in peritonitis, and worse, spiraling into sepsis. At the bedside, we performed a diagnostic peritoneal tap. The syringe filled with thick, purulent fluid—pus. Our worst fears were confirmed: a severe intra-abdominal infection.
Without delay, a pigtail catheter was inserted to begin draining the infected fluid. But the storm was far from over. He slipped into septic shock, requiring escalating doses of inotropic support just to maintain perfusion. His breathing worsened, necessitating ventilatory support. Meanwhile, his kidneys—already struggling—gave in, and continuous haemodialysis was initiated to manage the acute kidney injury.
Gradually, and against the odds, he started to improve. For a brief moment, hope found a foothold in our ICU.

The Diagnosis That Changed Everything:
The biopsy results came in—Gastrointestinal Stromal Tumor (GIST). It had already spread extensively, wrapping itself around local structures and ruling out the possibility of surgical cure.
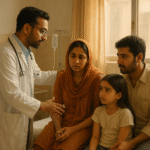
We sat with the family, explained the situation with clarity and compassion, and brought in our oncology colleagues. Chemotherapy was initiated to slow progression and relieve symptoms.
The Next Hit:
During his ICU stay, just as we were beginning to stabilize him, another crisis struck—a sudden, massive gastrointestinal bleed. Blood pressure plummeted, his hemoglobin dropped drastically, and we found ourselves racing against time once again.
Given his critical condition and the extensive local spread of the underlying tumor, surgery was no longer an option. We urgently called upon our interventional radiology team. Imaging revealed active bleeding from the inferior gastric artery. With precision and speed, the artery was successfully embolized—buying us precious time and a fragile stability.
When the Disease Fights Back:
Despite our relentless efforts, the tumor showed no signs of retreat. It continued its silent, aggressive march—eventually eroding into the small intestine. The resulting complications left us with no choice but to proceed with a palliative debulking surgery, followed by the creation of a loop colostomy. It was a difficult decision, made with the hope of easing his suffering, not curing the disease.
But even after surgery, his condition never truly stabilized. His body, already weakened by sepsis, shock, and multi-organ failure, couldn’t bounce back. The disease had exacted a toll beyond repair—one that no medicine or intervention could reverse.

A Quiet Farewell:
The patient’s children, who came from a small town with limited understanding of medical complexities, showed remarkable resilience. Despite the emotional and financial strain of prolonged ICU care, they clung to hope for nearly a month—trusting the care process, praying for recovery, and standing by their father through every uncertain moment.
As the clinical reality became clearer, we engaged in several open and compassionate conversations with them. By then, they had walked this journey closely with us—witnessing the struggles, the fleeting victories, and the steady decline. It was a deeply emotional and difficult process, but with continued support and understanding, they made a brave and humane decision: Do Not Resuscitate.
It wasn’t a decision to give up—it was an act of love. A choice to let go with dignity.
He passed away peacefully. A warrior who fought till the end. A soul who reminded us of the fine line between life and death, between science and surrender.

Reflections from the ICU:
Every doctor carries certain cases with them—etched not in files but in memory. This was one of them. We lost him not because he taught us about grace in suffering, the strength of families, and the silent resilience of the human body and spirit.
“As an intensivist, getting lost in numbers, machines, and protocols is easy. But this case reminded me why I chose this path—to stand beside my patients, especially when the path ahead is uncertain.”